The increasing presence of private hospitals has brought an era of better healthcare services in Nepal despite several challenges.
--BY SANJEEV SHARMA
Access to healthcare for the average Nepali has significantly improved in the last three decades. The increasing availability of better healthcare services in the country has led to a rise in almost all health related indicators. The Life expectancy of Nepalis, for instance, currently stands at 68.19 years which was 54.20 years in 1990. Similarly, the death rate per 1,000 people in Nepal has halved to 6.3 in 2015 from 12.9 in 1990.
Other health indicators such as maternal mortality, infant mortality and child mortality have also notably improved over these years clearly signaling that Nepalis at present are receiving better healthcare services than before. The improvements in the healthcare services have reflected in the Human Development performance where Nepal has ranked 144 in the 2016 Human Development Index (HDI) with a HDI value of 0.558 compared to 0.378 in 1990.
Thanks to the increasing presence of private healthcare service providers, Nepal has been marching ahead to become a healthy country in the 21st century. Given the current scenario of healthcare in the country, Nepali private healthcare service providers have been playing a very important role in terms of increasing access to healthcare and accelerating the Universal Healthcare Coverage which is one of the goals of the Sustainable Development Goals (SDGs), a collection of global targets set out by the United Nations for its member nations to achieve by 2030 starting from the year 2016. They are effectively providing treatments for various types of general aliments, life-threatening diseases and carrying out complex surgeries to solve different health related issues saving the precious lives of millions of Nepalis.
“The healthcare service in Nepal is moving in the right direction now,” observes Dr Chakra Raj Pandey, managing director of Grande International Hospital. He sees a bright future for the sector as healthcare services in the country have become more advanced with the time.

Healthcare Sector in Nutshell
- Health spending per capita- USD 39.87 (2014)
- Total expenditure on Health per capita USD 137 (2014)
- 0.67 doctors and nurses, 0.9 hospitals per 1,000 population(WHO recommendation- 2.3 doctors, nurses and midwives per 1,000 population)
- 61.8 percent of the households in Nepal have access to health facilities within 30 minutes.
- 63 percent patients with acute illness preferred private healthcare centers to public hospitals.
- FDI of about USD 19 million since 2008.
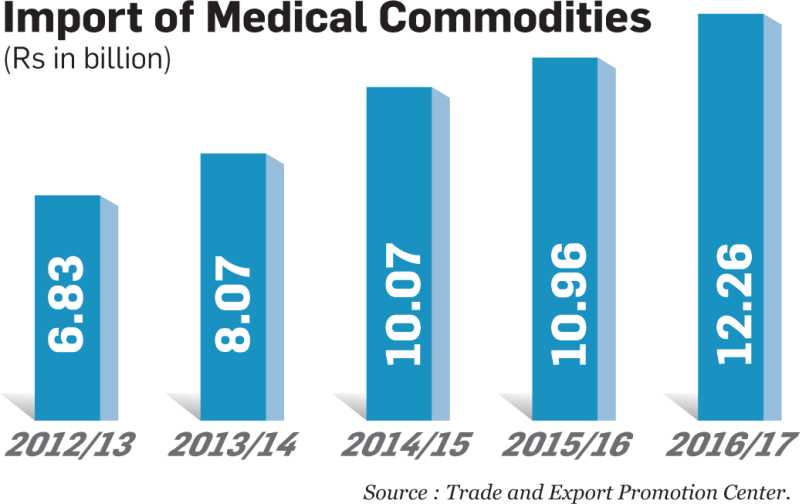
- Import of medical commodities doubled from Rs 6.83 billion in FY 2012/13 to Rs 12.26 billion in FY 2016/17.
The Booming Healthcare Industry
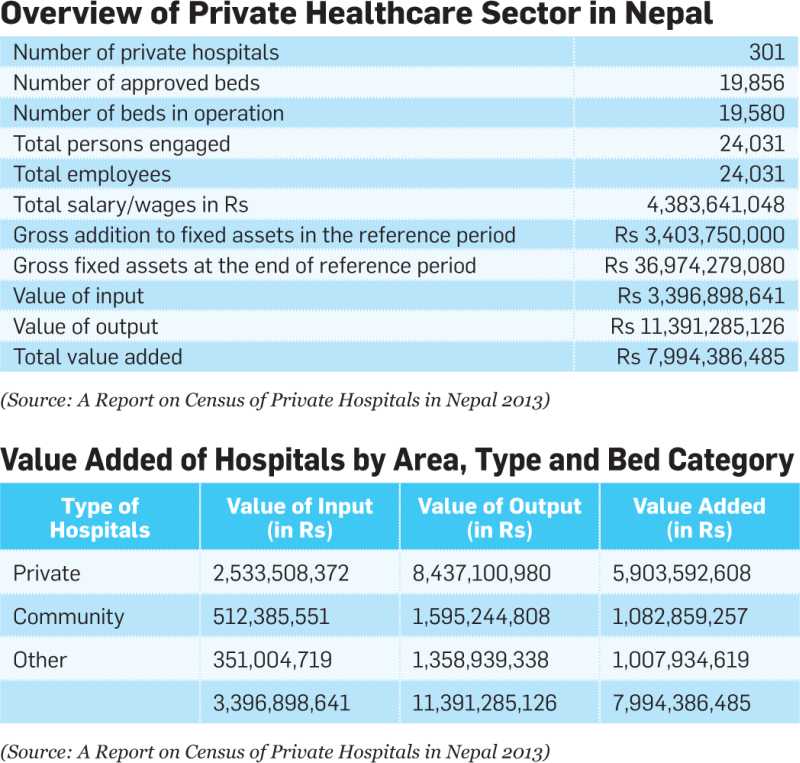
It is the private healthcare institutions which have helped establish the concept of holistic and invasive healthcare services in Nepal by introducing latest techniques and equipments in treatment. After the political changes of 1990 the attraction of private investors towards the country’s healthcare sector began to rise. Supported by the government’ policy of economic liberalisation, the sector saw massive investment with the opening of hundreds of private hospitals over the period of 27 years. According to the Central Bureau of Statistics (CBS), 301 private hospitals are active in the country at present, whereas the number was a mere 16 in 1990. However, according to the data published by the Association of Private Health Institutions in Nepal (APHIN), the umbrella organisation of Nepali private hospitals, there are 400 hospitals in the country out of which 200 are privately-owned. “Currently, there are 200 private healthcare service providers out of which nearly 160 comes under the APHIN’s umbrella,” says RP Mainali, deputy general manager, PR and Publicity/Corp. Communication at Norvic International Hospital.
Though the actual market size of the domestic healthcare sector is unknown due to lack of authentic data, Mainali estimates the total market size of private sector hospitals to be over Rs 20 billion at present with a total bed strength of approximately 15,000compared to 7,000 beds of government-run hospitals.
The sharp rise in the number of hospitals has ultimately resulted in a large healthcare industry where thousands of doctors, nurses, technicians and other health professionals are working. Similarly, the industry has also employed a large number of professionals in the areas of human resource management, accounts, finance and procurement, among others, to look after the corporate objectives of the healthcare institutions.

According to APHIN, about 16,000 professionals are employed by the domestic private hospitals in both technical and non-technical areas. Similarly, a 2014 CBS report shows that a total of 24,031 staff have been employed in the private healthcare sector. The Nepal Health Sector Support Programme, a joint initiative of the government of Nepal and UKAid, estimates that the private healthcare industry employs about 60 percent of doctors in Nepal. Similarly, private hospitals cover over two thirds of the hospital beds in the country, according to a report published by the Ministry of Health in 2012.
Among the long list of private hospitals in Nepal are Norvic, Grande, B&B, Om, Kathmandu Medical College, Manipal Medical College, Vayodha and Medicare who established themselves as the major multi-specialty healthcare centres by building a strong level of trust among Nepalis through quality service. The success of these hospitals has clearly shown the business potential in the healthcare sector, thus drawing the attention of both local and expatriate Nepali investors. The private healthcare sector over the years has observed a slew of institutional investments with major business houses getting attracted towards it. The establishment of the Norvic Health Care and Research Center (now Norvic International Hospital) by the Chaudhary Group in 1994 is considered as a stepping stone in this regard. Since then, hospitals including Om, Medicare, Kathmandu Medical College, Grande International, Vayodha, and Neuro, among others, have all started with institutional investments.
Adding to the list is the newly opened Nepal Mediciti Hospital which aims to become the ‘super multi-specialty’ healthcare centre in Nepal providing all types of medical services to patients. “A total of almost Rs 8 billion has been invested to build this hospital,” informs SudhakarJayaram, CEO of Nepal Mediciti. The hospital situated at Sainbu, Lalitpur has been opened with the initiation of Nepali expat entrepreneur Dr Upendra Mahato and has perhaps the largest medical facility and infrastructure among the private healthcare centres in the country at present. “It doesn’t matter how big the infrastructure of the hospital is. We believe that every patient should get safe treatment and proper care. People should not think the infrastructure of the hospital is big so that the treatment in Mediciti will be costlier,” expresses Jayaram. He claims that the cost of treatment at Mediciti is almost 10 percent cheaper than that at other Nepali private hospitals.
Apart from the increasing number of multi-services healthcare centres, specialty hospitals are also being opened here. The Star Hospital recently started the Kathmandu Star Cancer Center at Sanepa, Lalitpur. In July, the 75-bed Nepal Cancer Hospital and Research Center situated at Harisiddhi, Lalitpur was officially inaugurated by President Bidhya Devi Bhandari. The hospital which covers an area of 24 ropanis of land has an investment of Rs 1.75 billion.
Nevertheless, there are also concerns among the stakeholders that the quality of the services can be compromised with the mushrooming of hospitals. “Operating a hospital is not just like running any other business. It should be kept in mind that running a health service organisation is very sensitive and risk bearing and the operators are required to be very sensible and responsible,” thinks Mainali.
Dr Pandey sees the increasing interest of the private sector in healthcare as good. “However, the government should regulate the health sector properly. Healthcare has to be linked with education. To provide good service to the people, the doctors should be highly skilled,” he says. According to him, every hospital has to update their medical professionals so as to continuously improve the quality of services.
Service Expansion
It is interesting to note that the goal of Nepali private healthcare service providers to keep themselves up-to-date with the latest global medical advancements has led to healthcare technology quickly arriving in the country. According to RP Mainali of Norvic, whenever new healthcare technology is launched in the west, the same is introduced (at least in the private sector hospitals) in Nepal within 30 to 60 days.
Private hospitals have been expanding their services with the most advanced diagnostic equipments and state-of-the-art facilities ensuring world-class treatment to patients. “We have started many services and now mostly we are in the process of refining those services. We will also be promoting the bypass surgery and interventional cardiology,” says Dr Pandey of Grande International Hospital, adding, “We want to go for in-vitro fertilisation very soon and we are also planning to expand the oncology department.”
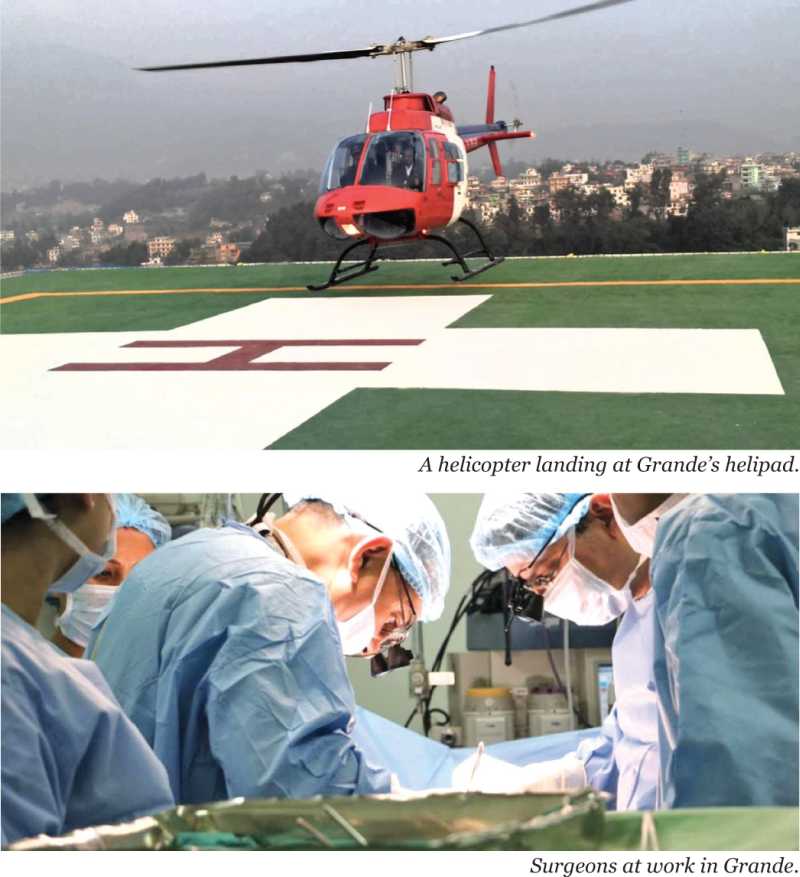
Norvic International Hospital is also going start a highly specialised mother and child care regime and IVF technology soon while dialysis services are also in the pipeline. “Norvic plans to further upgrade the diagnostic services to newer heights to convert the hospital into an international class nuclear medicine centre,” says Mainali. The expansion plans of the hospital also include increasing the bed strength to over 350 by adding 200 more beds in the near future, upgrading some of its super specialty centres such as Cardiology Centre, Digestive Disease Centre, Pulmonology Centre and Trauma Care Centre, and adding five more modular operating suites to the current three JCI standard modular operating suites. “The total new built up area will cover 132,000 square feet and the new infrastructure will also have a helipad,” shares Mainali.
Meanwhile, the newly established Nepal Mediciti currently has plans to increase the current bed strength of 300 to 550 within a year and to 750 within three years. It is also planning to commence a post-graduation medical programme within a year. “Unless we start a post-graduation programme, we will not be able to fulfill the supply of high quality medical doctors,” says Nepal Mediciti CEO Jayaram.
The presence of private healthcare service providers have resulted in the availability of top-class medical practices within Nepal, thus strengthening public trust in local hospital services and reducing the outflow of money from Nepal in terms of receiving medical treatments abroad. “We are retaining almost 1.32 billion rupees a year that would have gone abroad in the absence of quality treatment services in Nepal,” says Dr Pandey. “Patients coming here whether they are from well-to-do families, middle class or lower class families feel good about the services here.”The fact that a majority of patients in the country choose private hospitals clearly indicates the level of confidence of the general public in the private healthcare services. The Nepal Living Standard Survey 2011finds that about 63 percent of patients with an acute illness, regardless of their economic status, have gone to private hospitals for treatment.
Growing Partnership
In recent years, Nepali private healthcare service providers have been joining hands with local and foreign partners to open new hospitals and introduce new medical technologies. The newly opened Kathmandu Star Cancer Center, for instance is one such venture, which is collaboration between the Star Hospital and Kathmandu Cancer Center. Similarly, Norvic and the Indian healthcare services major Medanta Medicity have been in collaboration since 2010 for transfer of technology and medical expertise.
Vayodha Hospital also has a tie-up with the Fortis Escorts Heart Institute, New Delhi since its commencement in mid-2012. Vayodha in July further expanded the association by opening the electronic intensive care unit (eICU) Critinext and a blood bank. According to the hospital, it is the first time that any hospital in Nepal has opened an eICU facility. In the meantime, Grande has partnered with Samitivej Hospitals of Thailand since 2011. “We are working as the consulting partner and are more involved in hospital management,” says Manish Bhadra, management representative at Nepal Representative Office of Samitivej Hospitals. “The services of our partners have definitely improved in comparison to when we were not involved,” he adds. Likewise, Om Hospital has partnered with the New Delhi-based Apollo Hospital for telemedicine and other areas.
Top 12 Causes of Deaths in Nepal
1. Ischemic heart disease
2. COPD (Chronic obstructive pulmonary disease)
3. Cerebrovascular Diseases
4. Lower respiratory infect
5. Diarrheal Diseases
6. Diabetes
7. Neonatal Encephalopathy
8. Road injuries
9. Chronic Kidney Disease
10. Tuberculosis
11. Asthma
12. Other Neonatal
(Source: Institute for Health Metrics and Evaluation, University of Washington, Seattle)
Problems
Despite the promising growth of the industry and best efforts of the service providers in delivering quality medical services to Nepalis, the sector also faces a number of problems. From the safety of doctors and health professionals to difficulties in import of necessary medical equipments and commodities, there is a long list of issues to be addressed. Safety issues concerning doctors, health professionals and medical facilities have become one of the most concerning matters in the healthcare sector, mostly over the last decade. Over the years, there have been physical attacks on doctors, nurses and other staff and destruction of hospital properties in alarming numbers by hooligans in case of patient deaths during medical treatment creating an atmosphere of trepidation among the healthcare professionals.
Though the attacks have declined over the last few years, such incidents still occur sporadically. Dr Pandey says doctors are not gods and there are cases where even the doctors cannot do anything. “Doctors have to be protected because they don’t have bad intention towards their patients. However, the hospitals have to be safe and the learning should be advanced,” he mentions. He urges that the disputing sides need to sit and resolve the issues through talks in case such problems arise. He also stresses for a legal framework to address such problemsat the government level.
Similarly, Mainali sees the occurrence of such incidents as a result of poor education, low morale and lack of discipline and implementation of proper rules and regulations pertaining to the subject. “The concerned government authorities must ensure the safety and security of doctors and health care professionals. Otherwise, the service providers will think twice when accepting patients who are in a critical state,” he opines. He is also of the view that the policy of ‘jail without bail’ must be implemented for anyone who threatens the healthcare professionals and vandalises the property of hospitals.
The low level of available highly qualified medical and technical manpower is also another major problem for private healthcare service providers. “There is a high human resource turnover and the problem of brain drain of the qualified manpower,” says Mainali. A study carried out by the Nick Simons Institute in 2012 estimates that 20-30 percent of 12,000 registered doctors in Nepal have been practicing abroad. According to the institute, 36 percent of the doctors who graduated from Tribhuvan University Institute of Medicine from 1983 to 2004 have moved abroad. It was also found that half of the 1,500 students graduating from medical schools in Nepal every year go to other countries in search of higher salaries and a better life. The study also observed a similar pattern of migration of nurses and pharmacists who graduated in Nepal.
Meanwhile, burdensome procedures in importing necessary medical equipments, commodities and peripherals also restrict the smooth operation of the hospitals, say stakeholders. “Almost all pieces of medical equipment are imported here, and the customs process is a nightmare,” shares Nepal Mediciti CEO Jayaram. According to Mainali of Norvic, the non-availability of necessary medical equipment, instruments and spare parts in the country along with poor after sales services and are also big problems. He suggests for a flexible customs duty structure on the import of high-end equipment and instruments.
“Second, the provision for importing such equipment from the country of origin should be reconsidered. For example, the country of origin of certain equipment is in Europe, but the same product is also available in the neighboring countries,” he says. “Hence, the importer should be given the right to purchase the equipment from the neighboring countries so as to ensure timely delivery of the life saving products.”
The very low penetration level of medical insurance is another major issue here. It is estimated that out-of-pocket medical expenditure of Nepalis accounts for over 81 percent of the total healthcare payments made in the country. “Insurance policies implemented to some extent do not have greater degree of penetration and hence every patient has to pay the expense from their pockets for the medical treatments,” says Mainali. Dr Pandey of Grande talks about the role of healthcare service providers in this regard. “We should also make the people aware about medical insurance,” he says. After a prolonged delay, the government in 2016 officially implemented the National Health Insurance Policy by starting health insurance for people in various districts of the country. The process which is ongoing is said to have been receiving a lukewarm reception from the general public. It is because of the confusion that prevails in terms of the insurance coverage as the government-run scheme does not fall in the purview of the Insurance Board, the insurance sector regulator.
Apart from this, the lack of subsidies for private healthcare service providers also is considered as a problem for the hospitals to grow and patients to receive services at relatively low costs. According to a 2014 Dolma Development Fund report, the private healthcare industry in Nepal has very few tax and subsidy incentives, and given the difficult nature of business, this can drive up prices for end consumers making healthcare services unaffordable.“Other developing countries often have specific incentives for private healthcare companies such as tax breaks for a certain period of time, subsidised land, and relaxation on import duties,” states the report. Citing neighbouring India as an example, the report says, “The government in India provides free land for 99 years to private hospitals in underserved areas, has relaxed import duties for several hospital projects, and does not tax revenues of hospitals with more than 100 beds for the first 5 years of their operations.”
The current corporate tax rate also contributes to the higher operational costs of the hospitals. The private hospitals are required to pay a statutory corporate income tax of 25 percent which is 20 percent for most types of businesses in the service sector. “We are in a service sector. So, the government should work on supporting the health sector to reduce the financial burden,” mentions Jayaram.
Lack of proper infrastructure and no proper control over malpractice in some parts of the country are other problems, according to stakeholders.
Mainali thinks the government should come up with sector-friendly policies that can encourage the workers while also making them responsible towards their business. “The government can play a pivotal role in forming a sort of consortium so that adequate funds can be created and high-end diagnostics facilities can be arranged,” he further suggests, adding, “Due to the lack of sufficient money, diagnostics in Nepal are restricted to medium range technology.”